In an ongoing effort to balance the needs of patients and their families with increasingly complex insurance requirements, Grays Harbor Community Hospital (GHCH) created a new Care Transitions Team last April.
The new team brings together social workers, utilization review (UR) nurses and clinical documentation specialists, functions that previously worked independently. Pulling these resources together under one roof allows for more effective coordination of care and better communication with insurers.
Social workers work directly with patients and their families to provide patient counseling, develop discharge plans, and in general act as a patient advocate. UR nurses continually monitor care to ensure that patients get the services they need and that insurance requirements are met. Clinical documentation specialists manage the medical record throughout the patient stay.
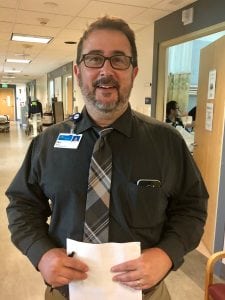
“This is about people entering into and moving through the healthcare system efficiently and appropriately,” explains Phil Royer, Director of Care Transitions. Royer’s team coordinates the continuum of care from admissions through patient stay and discharge. The goal is to provide patients the care they need and to ensure proper reimbursement from Medicare and other insurers.
The team was initially formed to meet two immediate needs. The first is effective discharge planning.
“The most visible way the Care Transitions team affects patients and families is in the discharge process,” states Royer. “They meet with a social worker who will talk with them about their situation. What supports do you have to call on? What’s missing? What additional resources do we need?”
Behind the scenes, UR nurses keep a clinical eye on the patient and their process to help anticipate the time of discharge and to head off any medical issues early on. Social workers, UR nurses, dieticians, the pharmacist, the charge nurse and sometimes providers or rehab services meet daily to review the patient’s case.
“There’s a team, coordinated by Care Transitions, that looks at the clinical care from every aspect, making recommendations and working with patients and their families,” says Royer.
A second goal of the team is to achieve appropriate patient classification and to make sure that clinical documentation gives an accurate picture of the care provided. UR and clinical documentation are critical to proper reimbursement, decreasing financial headaches for both patients and the hospital.
“Utilization is all about getting patients in the right status,” explains Royer. “Are they an inpatient, or are they an observation patient? Do they meet acuity? Communicating on the front end with payors is essential, so we’re working that relationship and checking all the right boxes. We’ve done simple things like setting up an insurance hotline so that we’re not missing calls.”
In fact, patient status and the way in which the information is documented can make a difference in reimbursement of tens of thousands of dollars on a single medical record. “It’s important to capture an accurate picture of the care being provided,” adds Royer. “For instance, are we just treating pneumonia, or are we treating bilateral pneumonia with sepsis?”
Patient status is essential to reimbursement and is based on complex national guidelines. Criteria for classification as inpatient or observation include the severity of the illness, the intensity of the services required, and the duration of stay. Generally, but not always, a stay of more than two midnights will result in inpatient classification.

“When we created the team, we realized that we didn’t have a good knowledge base regarding inpatient and observation status,” remembers Melanie Brandt, Chief Nursing Officer. “We provided extensive education on patient classification to ensure compliance to regulations. We are still on that learning path, still growing as a team.”
While the Care Transitions Team is meticulous about complying with Medicare regulations, they have not lost their focus on the patients. UR nurses watch over every step of the patient’s care, and social workers coordinate resources as the patient prepares to leave the hospital.
“It’s a very complex process, and in some cases it comes down to getting the right words in the right order in the right place,” says Royer. “It reflects a lot of the heartbreak of health care in our country, but to our hospital’s credit, we’ve always been in the business of doing the right thing.”
While it’s easy to lose track of the human element, the Care Transitions Team at GHCH helps to build a bridge between regulations and needs that reach beyond the medical. “Appropriate payment is super important,” acknowledges Royer, “but the heart of the hospital hasn’t been carved out.”
Learn more at the Grays Harbor Community Hospital website.
Sponsored
















































